Ann Roy Australas Coll Den! Surg 1998;14:70-4
ENDODONTIC TREATMENT: WHAT CAN AND WHAT CAN’T BE SAVED
David Figdor, MDSc, LDS, FRACDS(DipEndo)
|
|
Dr Figdor is in Specialist Endodontic Practice in Melbourne. He is a Senior Fellow, School of Dental Science, University of Melbourne as a part-time lecturer and clinical teacher in endodontics. He is also a visiting scientist in the Department of Microbiology, Monash University, and has lectured widely locally, nationally and internationally. He has authored and co-authored numerous papers and is the co-author of a chapter in a new textbook on endodontics. |
ABSTRACT
Although endodontic treatment is generally considered to have a high success rate, not all teeth provide an opportunity for predictable salvage by endodontic therapy and subsequent restoration. New studies are yielding valuable information about factors that affect the outcome of treatment, which enhances the ability of the clinician to make a more accurate preoperative assessment and improve the quality and predictability of treatment.
Most teeth can be saved by endodontic treatment; however, some cases fail despite good treatment. How can we assess and predict the outcome of treatment? This paper reviews reasons for biological failure of endodontic treatment and describes clinical factors that influence whether you might treat, refer, or extract the tooth.
INTRODUCTION
Many clinicians are faced with daily dilemmas about whether damaged teeth can be salvaged (Fig. 1). The aim of this paper is to review success rates, integrate new information about the limitations of endodontic treatment, and describe factors to consider in determining whether a general practitioner can reasonably treat the case.
It is critical that the essential role of microorganisms in the development of the periapical lesion be understood. This is because infection is by far the prime cause of endodontic disease and the outcome of endodontic treatment depends on control of this problem. We know from animal and human studies that bacteria are essential for the development of periapical disease.1-3 Whether or not an inflammatory lesion at the root apex will resolve depends on our ability to remove microorganisms from the root canal during endodontic treatment. All of the scientific data are consistent with empirical clinical experience, which shows that if you control infection in the canal, periapical healing will follow.
Even small numbers of bacteria that persist in the root canal at the time of root filling have a significant influence on the outcome of treatment. In a recent study, the importance of infection at the time of root filling on the prognosis for treatment was revealed.4 When bacteria could be recovered from the canal at the time of root filling, the success rate was 26 per cent lower than for those teeth in which no bacteria were recovered at the time of root filling.4 This implies that whenever bacteria are present, there is always a risk that they may survive and continue to inflame the periapical tissues.
So, the short answer to the question ‘What can be saved?’ is that if you can remove bacteria from the root canal system, you have a good change of saving the tooth; but many clinical cases are more complex than that.
SAVING TEETH – A CONTINUUM
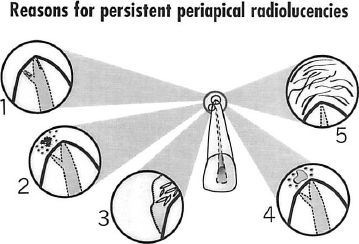
I would like to put to you the concept that ‘What can and what can’t be saved’ is actually a continuum (Fig. 2). You might imagine the problem as a walkway with one end on safe, firm ground and the other end precariously balanced and unsupported. At one end of the walkway, represented by that on secure ground, certain teeth can be saved with a very high probability of success. At the other end, represented by the precariously balanced part of the walkway, there are some teeth that definitely cannot be saved.
The area of most interest and challenge is a grey zone, roughly in the middle. That is where difficult decisions must be made about whether or not the tooth can be saved. In a paradoxical way, the more you approach the centre and try to define where the tooth is in this grey zone, the harder it is to determine or predict the outcome of treatment.
It seems reasonable to assume that the vast majority of teeth fall into the category represented by the walkway on secure ground, that is teeth that can be saved. What I shall address as we transverse the walkway are two main areas. Firstly, what are the limitations of our success rate from a biological point of view? Secondly, what clinical factors help you to determine whether you might treat, refer, or extract the tooth?
SUCCESS RATE
Let’s start by looking at success and failure of endodontic therapy. The vast majority of teeth can be saved by endodontic treatment when it is performed to accepted clinical standards.5,6 Most long-term, follow-up studies report success rates of about 90 per cent for endodontic treatment.5,6

Fig. 1.–Example of an upper right premolar in an apparently precarious situation. a. No root filling is evident, the canals are calcified, there is a large bulky post with a near perforation and a periapical area. b, Nevertheless, this case could be salvaged by removal of the post and crown, finding and cleaning two canals and root filling. c. Healing is evident six months later, following which the tooth could be restored.
There are some key factors that affect the outcome of endodontic therapy. The preoperative status affects the success rate, so that vital teeth have a 96 per cent success rate compared with teeth with a preoperative periapical lesion that have a success rate of 86 per cent.7 There is general agreement that if the instrumentation and root filling is 0-2 mm from the root apex, then the prognosis is good. There is a reduced prognosis for overfilled teeth with preoperative periapical lesions.7 A third factor is that there is an upper ceiling to the success rate,7 which means that it is not possible to achieve a 100 per cent success due to biological factors, and this is addressed in more detail below.
BIOLOGICAL FACTORS THAT AFFECT THE OUTCOME OF ENDODONTIC TREATMENT
Inadequacies in root canal obturation have been frequently blamed for failure of endodontic treatment. Whilst a high standard of root canal obturation is a clinical goal of treatment, it is incorrect to assume that poor obturation is in itself the cause of failure.8 The prime aetiological factor responsible for most failures is residual or persistent infection of the root canal, rather than the quality of the root filling. However, a poorly filled canal can jeopardize the integrity of the periapical tissues because bacteria may have an opportunity to infect the canal via leakage around the coronal restoration.
It should be emphasized that most failures are due to technical problems that occur during treatment, particularly where the root canal infection is not adequately controlled by the clinical procedures applied to the tooth. These types of failure are not addressed here.
When endodontic treatment has been well performed, there is still a small proportion of cases that fail. This implies that there is an upper ceiling to the success rate since some factors may influence the outcome, which are beyond the control of the patient or clinician.
In a series of studies that have analysed the reasons for failure, four reasons for biological failure have been identified. These include persistent intraradicular microorganisms,9 extraradicular infection,10,11 extraradicular foreign material12 and true cysts especially those containing cholesterol crystals.13
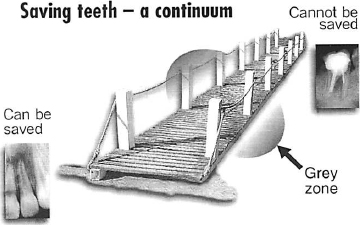
Fig. 2.–The problem of saving teeth can be regarded as a continuum, represented as a path or walkway. At one end, bottom left, teeth can be saved with a high change of success and at the other end, top right, some teeth cannot be saved. The most challenging clinical decisions are in a middle, grey zone where the outcome of treatment is uncertain.
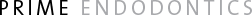
Fig. 3.–Reasons for persisting periapical radiolucencies when endodontic treatment has been performed to a high standard include: 1, Intraradicular microorganisms in unfilled spaces in the canal; 2, Extraradicular infection; 3, True cyst with cholesterol crystals; 4, Extraradicular foreign material; and 5, Healing by fibrous scar tissue.
Recently, a fifth factor associated with persistent periapical radiolucencies has been identified.14 This study examined cases in which the endodontic treatment had been performed to a high standard, but on follow-up there was a persistent periapical radiolucency.14 When correlative light and electron microscopy was performed on the biopsies, two cases involved an intraradicular infection, one case was a cyst, and two cases revealed fibrous scar tissue healing following conventional treatment. This means that in rare cases a persistent radiolucency may be misinterpreted as a failure when the periapical lesions heals with fibrous scar tissue.
In summary, there are five reasons for persistent periapical radiolucencies when everything has been done to a high standard (Fig. 3). These are:
1. Intraradicular microorganisms in unfilled spaces in the canal.
2. Extraradicular infections caused by actinomyces and propionibacterium species.
3. Extraradicular foreign material.
4. True cysts with cholesterol crystals.
5. Healing by fibrous scar tissue.
CLINICAL FACTORS
Before commencing treatment, careful case assessment is important to ensure the best possible outcome of treatment and a less stressful course for both the clinician and patient. The clinical assessment is based on integrating the history. examination, tests and radiographs to arrive at a realistic judgement about the prognosis for the tooth. In evaluating risk, the main factors can be divided into three groups: general, local dental, and endodontic factors. The features outlined within each group are clinically significant, but this is not an all-inclusive list.

Fig. 4.–Example of a tooth compromised by destruction of the crown by caries. Endodontic therapy is not warranted on tooth 47 since restorative treatment is not possible.
General factors
There are few general factors that mitigate against a successful outcome of endodontic therapy: however, two factors may complicate the treatment process.
1. Medical factors
Most of the medical factors that impact on general dentistry have a similar bearing on endodontic treatment, such as potential drug interactions and the requirement for an antibiotic cover in selected cases. Relatively few factors present a special problem in endodontics although some medical conditions, such as diabetes, can involve impaired tissue healing and may therefore warrant extra care and skill provided by a specialist endodontist.
2. Patient cooperation
This is an occasional complicating factor that can compromise treatment. For example, anxiety problems, difficulty in opening the mouth or in reclining the patient may necessitate referral to an endodontist.
Local dental factors
1. Diagnosis
Difficulties in arriving at a diagnosis are a common reason for referral. This is especially so when the patient presents with diffuse or radiating pain, the source of which can be challenging to identify.
2. Local anaesthesia
This is a common problem, particularly in the lower molar area where anaesthesia depends on the often unreliable inferior alveolar nerve block. The problem can be aggravated when the molar tooth has a ‘hot pulp’, in which a seemingly effective nerve block is ineffective for the proposed pulp extirpation.

Fig. 5.–Tooth 37 has a severe mesial inclination which compromises the access cavity for endodontic treatment.
3. Periodontal status
Prior to commencing treatment, it is essential to assess the periodontal support available. If the periodontal attachment is insufficient, then no amount of endodontic treatment can save the tooth. When doubt exists about the periodontal prognosis, a periodontist should be involved in assessment of the tooth prior to treatment.
4. Restorative status
It is important to ensure that there is sufficient tooth structure available so that the tooth can be restored after endodontic treatment. Almost any tooth can technically undergo endodontic treatment, but it must have sufficient tooth structure available for restoration at the completion of endodontic treatment (Fig. 4).
Endodontic factors
1. Radiographs
If you cannot get accurate radiographs before and during treatment, it is difficult to perform treatment properly. The dental or oral anatomy may present a challenge to accurate radiography, but of equal importance are simple measures such as correct film processing.
2. Root and canal morphology
It is essential to carefully assess the tooth anatomy, especially the curvature and lateral dimensions of each root and the number, narrowness and curvature of each canal before embarking on treatment. Many procedural errors that have occurred during treatment could have been avoided if these anatomical facts were recognized prior to treatment.
3. Pulp space
Most general practitioners will recognize the narrow, calcified canal as a problem: however, in the hands of a specialist endodontist, about 80 per cent of these calcified canals can be successfully located and negotiated. A less well anticipated problem is the narrow, calcified pulp chamber in molar teeth. This can make it difficult to locate the canals and may result in a furcation perforation during the search for the canals.
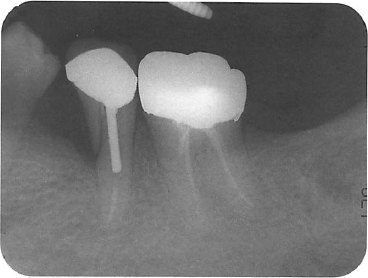
Fig. 6.–Lower left premolar with a deep crack extending into the tooth root. The prognosis for this tooth is poor.
4. Tooth position or inclination
Occasionally, it is very difficult to reach a tooth in some mouths; or a tooth may be unusually long or tilted, which makes access and visibility poor (Fig. 5).
5. Cracks
This is a complex issue since there are many different types of cracks in teeth and a wide spectrum of presentations and outcomes are possible. Briefly, if a tooth is split vertically then the prognosis is very poor (Fig. 6). However, incomplete cracks in the crown of a tooth may be treatable depending on the nature, location and depth of the crack.
6. Canal obstructions
Occasionally canals may be obstructed prior to commencing treatment, for example, by a pulp stone. But by far the most common blockage is the iatrogenic obstruction that occurs during treatment. Fractured files and posts, ledging and blockage by dentine filings packed into the canal present a significant challenge to successfully completing treatment. Naturally, the best treatment is prevention!
7. Pathological factors
Some pathological entities can adversely affect the prognosis for the tooth. For example, root resorption may destroy significant amounts of tooth structure or create defects that communicate with the gingival crevice.
8. Iatrogenic complications
These usually require more complex treatment, frequently involving surgery in conjunction with re-treatment. A common example is an apical perforation that occurs during the practitioner’s attempts to clean a curved canal with large, straight instruments.
CONCLUSION
Many factors that influence the outcome of treatment have been identified in long-term follow-up studies. Whilst this information is useful for anticipating the prognosis of endodontic treatment, there is a limit to the precision of defining the outcome of an individual case. Although most endodontic treatment is a highly predictable procedure, predictability itself is a continuum in which many variables play a role. When assessing what can and what can’t be saved, the dentist must decide whether to treat, refer or extract. The answer varies with each case, but depends on the tooth, the patient and the knowledge and skill of the dentist. It is critical to carefully assess each case prior to starting treatment.
REFERENCES
1. Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol 1965;20:340-9.
2. Sundqvist G. Bacteriological studies of necrotic dental pulps. Umeå, Sweden: University of Umeå, 1976. Umeå University Odontological Dissertations No. 7.
3. Möller AJR, Fabricius L, Dahlén G, Öhman AE, Heyden G. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scan J Dent Res 1981;89:475-84.
4. Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J 1997;30:297-306.
5. Strindberg LZ. The dependence of the results of pulp therapy on certain factors. An analytical study based on radiographic and clinical follow-up examinations. Acta Odontol Scand 1956;l4(Suppl 21): 1-174. Dissertation.
6. Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod 1990;16:498-504.
7. Sjögren U. Success and failure in endodontics. Umeå, Sweden. University of Umeå, 1996. Umeå University Odontological Dissertations No. 60.
8. Sundqvist G, Figdor D. Endodontic treatment of apical periodontitis. In: Ørstavik D, Pitt Ford TR, eds. Essential endodontology. London: Blackwell Science, 1998:242-77.
9. Nair PNR, Sjögren U, Kahnberg K-E, Sundqvist G. Intraradicular bacteria and fungi in root-filled asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod 1990;16:580-8.
10. Sjögren U, Happonen RP, Kahnberg K-E, Sundqvist G. Survival of Arachnia propionica in periapical tissue. Int Endod J 1988;21:277-82.
11. O’Grady JF, Reade PC. Periapical actinomycosis involving Actinomyces israelii. J Endod 1988;14:147-9.
12. Nair PNR, Sjögren U, Krey G, Sundqvist G. Therapy-resistant foreign body giant cell granuloma at the periapex of a root-filled human tooth. J Endod 1990;16:589-95.
13. Nair PNR, Sjögren U, Schumachaer E, Sundqvist G. Radicular cyst affecting a root-filled human tooth: a long-term post-treatment follow-up. Int Endod J 1993;26:225-33.
14. Nair PNR, Sjögren U, Figdor D, Sundqvist G. Persistent periapical radiolucencies of root-filled human teeth include failed endodontic treatments and periapical scars. Oral Surg Oral Med Oral Pathol 1999 (in press).
Address for correspondence:
Medical Centre,
517 St Kilda Road,
Melbourne, Victoria 3004,
Australia.
Presented at the Fourteenth Convocation, Royal Australasian College of Dental Surgeons, Adelaide, October 1998.